Unrealistic Expectations?
Goals of care conversations are an essential and frequent (in some cases daily) part of our work as frontline clinicians.
While goals of care can relate to any medical treatment or management plan, the phrase has come to be aligned with discussions about the type of treatments doctors might offer if a person were to become suddenly so sick that they might die. People receiving healthcare might hear any number of terms to describe this process, most common are resuscitation or cardiopulmonary resuscitation (CPR), and there are many phrases to describe the decision-making process, Goals of (Patient) Care or DNACPR being some of the most common.
It’s fair to say these conversations are emotionally challenging all round, after all they are about life and death. Sometimes, we clinicians avoid these conversations until it’s too late to find out what’s most important to the person, to guide us with recommending the approach that would best fit with their values.
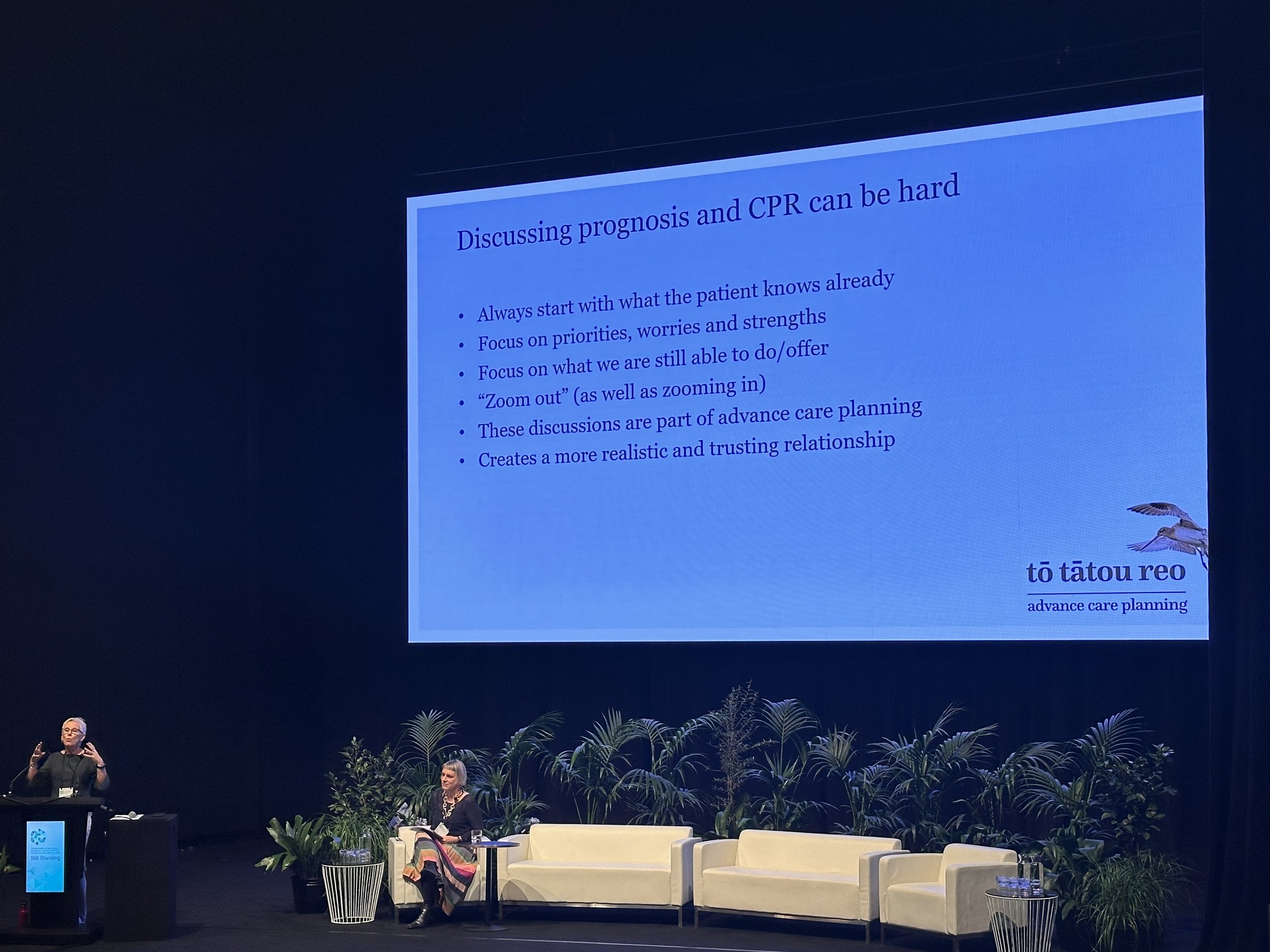
Kate Grundy and Jane Goodwin present their tips on discussing prognosis and CPR at ANZSGM 2024 conference, Ōtautahi Christchurch, Aotearoa New Zealand.
Reflecting on a recent conference I attended ANZSGM 2024 in Aotearoa New Zealand, I really enjoyed the insights of Jane Goodwin (Senior project manager – Te Tahu Hauora Health Quality & Safety Commission, To tatou reo advance care planning programme) and Kate Grundy (Palliative Care Specialist) on their approach to Shared Goals of Care conversations for Advance Care Planning (1). The work builds on the Serious Illness Conversation Guide a useful resource of patient-tested language for discussing goals of care.
These speakers introduced a phrase “Hope for the best, prepare for the rest” which resonates with my approach to discussion goals of care. Its also the title of a book by Sammy Winemaker and Hsien Seow (2).
Listening to the speakers’ experiences over decades of having, and training people in these conversations made me reflect on the subjects raised by doctors-in-training in my own teaching sessions on goals of care conversations.
Unrealistic expectations? Or an opportunity to connect
In teaching sessions I usually start by asking those present what they find challenging, and what they would want to talk about or would like help with.
One common question I hear is
“What do I do if there are unrealistic expectations?”
In fact I’m asked this nearly every time. The unspoken fear is often that the person may be hoping for treatments which, for their situation, have very little chance of survival let alone a good recovery.(3)
Let’s dig into this a little, what could it reveal?
Say you are about to have a goals of care conversation. Imagine yourself in the shoes of the person you are talking with, that might be your patient, or their medical treatment decision maker, who is likely to be one of their loved ones.
What might influence their expectations?
We’ve never known more about health and medical science
It can feel like everyday new medical discoveries are reported in the news
Medical dramas suggest that the chances of survival after a cardiac arrest are higher than in real-life (4,5) and all this regardless of the underlying health of the person
Ageing, death and dying are relatively taboo subjects (unless we are talking about avoiding them). Talk of the normal dying process of is rare.
Concepts such as clinical frailty are relatively new outside their medical contexts, and the impact of frailty on outcomes is not widely discussed (and frailty might sound more like a negative judgement rather than a clinical syndrome).
There are many more things that might factor into their expectations, including previous health care experiences, previous goals of care discussions their hopes and fears, their sense of responsibility…
Given all this messaging is it really unrealistic for them to expect and hope for the most intensive options?
Younger (6) and older people (7) have been found to have more optimistic views of outcomes of CPR. These views appear influenced by CPR depiction in medical dramas and at least in one study these are not mitigated by having had healthcare experience of training in or delivering CPR.(6)
Supporting Goals of Care Conversations
Where there is a mismatched agenda (patient’s and doctor’s not aligned), it is more likely a sign of how far apart our understanding of the current situation is.
In other words, it’s valuable data telling us what we need to do next. We need to bring our understanding together. As clinicians we can support this through questions exploring their goals, values and understanding , giving information where needed, and responding to our patient’s cues or emotions throughout. It is a powerful experience to be able to support this process well.
In my view, our work as doctors as clinicians guiding this conversation is to
Invite the person to have the conversation in a way that is clear and kind
Build a relationship that enables talking and listening about life and death, and emphasises our support and care, whatever may come.
Find out what the person already understands about their health issues, and what values are important to them in living well
Provide any context or information they might need from us
Combine understanding of what they would prioritise if they were sick enough that death is near, with our knowledge of what treatments and care would help in those situations
Communicate and document the outcome of the discussion so that all this information is available if (when) goals of care are next discussed.
The obvious benefits of doing this work, are coming to a shared understanding, and a clear plan, before a health crisis robs the person or their loved ones of the opportunity to be part of this conversation. There is also an additional benefit in building trust for future conversations, for a journey we will all make eventually in one way or another. We can support hope for the future, and aim for the right care for this person, at the right time.
I often end these discussions thanking the person for sharing their thoughts wth me, acknowledge it is not an easy topic to talk or to think about. I might say:
“Whatever happens, (or whatever comes) we will support and care for you”.
“We hope for the best, and prepare for everything”.
I say this because it’s what I would want to hear (and it’s the care I would want to have) in the same position.
Goodwin, J et al., Achievements and challenges during the development of an advance care planning program. AJA. 202140. 10.1111/ajag.12945.
Seow H and Winemaker S. (2023) Hope for the Best, Plan for the Rest: 7 Keys for Navigating a Life-Changing Diagnosis.
Bitter CC, Patel N, Hinyard L. Depiction of Resuscitation on Medical Dramas: Proposed Effect on Patient Expectations. Cureus. 2021 Apr 11;13(4):e14419.
Ramirez L et al., Cardiopulmonary resuscitation in television medical dramas: Results of the TVMD2 study. Am. J. Emerg. Med. 2021;43:238-242)
Bandolin NS, Huang W, Beckett L, et al Perspectives of emergency department attendees on outcomes of resuscitation efforts: origins and impact on cardiopulmonary resuscitation preference Emergency Medicine Journal 2020;37:611-616.
Zijlstra TJ, et al., Knowledge and preferences regarding cardiopulmonary resuscitation: A survey among older patients. Patient Educ Couns. 2016;99(1):160-3.